Evidence Based Medicine
A scientific approach for organizing and applying existing data to improve healthcare decisions. This involves integrating the best available evidence with clinical expertise and patient preferences to arrive at the best medical decision for the patient.
This section provide links to summaries of academic literature and references supporting interventions in Excell Physical Therapy characterized by their high safety and efficacy profile.

Exercise
INTRINSIC MECHANOTHERAPY
Therapeutic exercises enhance patients’ physical condition, restore function, prevent injury, and promote well-being through personalized programs designed to follow specific principles. Engaging in physical activities triggers physiological responses through the sympathetic nervous system, addressing increased demands during movement. Exercise impacts cardiovascular, neurological, and muscular systems. The cardiovascular system heightens heart rate and blood flow, enhancing endurance and heart health. Neurologically, exercise releases endorphins, dopamine, elevating mood and aiding cognitive function. Muscles adapt, becoming stronger and more efficient, while bones remodel, reducing fracture risk. Controlled stress initiates progress, improving performance and growth. Exercise positively affects metabolism for weight and metabolic health. It’s a holistic mechanism, maintaining internal equilibrium, enhancing overall health, and showcasing the body’s adaptability and vitality.
Learn More
Manual Therapy
EXTRINSIC MECHANOTHERAPY
A structured approach to delivering hands-on physical therapy within a biopsychosocial framework. Through mechanotransduction, mechanical forces are converted into biochemical signals within cells, tissues, or organisms. It is a fundamental physiological mechanism that allows cells to sense and respond to mechanical cues from their environment. This is administered to manage musculoskeletal conditions involving skilled movements and pressure to treat soft tissues and joints, aiming to improve mobility, reduce pain, and enhance overall function. It includes thorough assessment and personalised treatment plans based on patient-specific conditions. Mobilization involves gentle stretching of tissues, manipulation is a more forceful technique applied to joints, and massage targets muscles for relaxation and pain relief. It requires an in-depth comprehension of academic literature, anatomy, pathophysiology and patient response.
Learn More
Electrotherapy
Electrotherapy involves the application of electrical currents for therapeutic purposes mainly pain modulation, expedited tissue healing and neuromuscular reeducation. It requires understanding parameters like frequency, intensity, and waveform, which allows personalized programs that significantly influence treatment outcomes. It is based on high grade research and clinical reasoning. When applied correctly, electrotherapy holds a valuable role in clinical practice. Optimal outcomes hinge on the careful selection of modalities and dosages, underscoring their pivotal role in clinical decision-making.
Learn More
Thermogenesis
The application of heat for therapeutic purposes increases superficial and deep blood flow, accelerating tissue healing. Deep heating enhances collagen extensibility, reduce muscle spasms, decrease soft tissue viscosity and joint stiffness. Localized vasodilation increases metabolic rate and oxygen delivery promoting the removal of waste products and hastens healing processes. Heat’s relaxing effect on muscles is valuable in preparing for stretching exercises and improving range of motion. It can alleviate pain by reducing nerve excitability and sensitization. It requires a thorough understanding of thermodynamics including factors like heat absorption, stabilization, duration, and patient comfort.
Learn More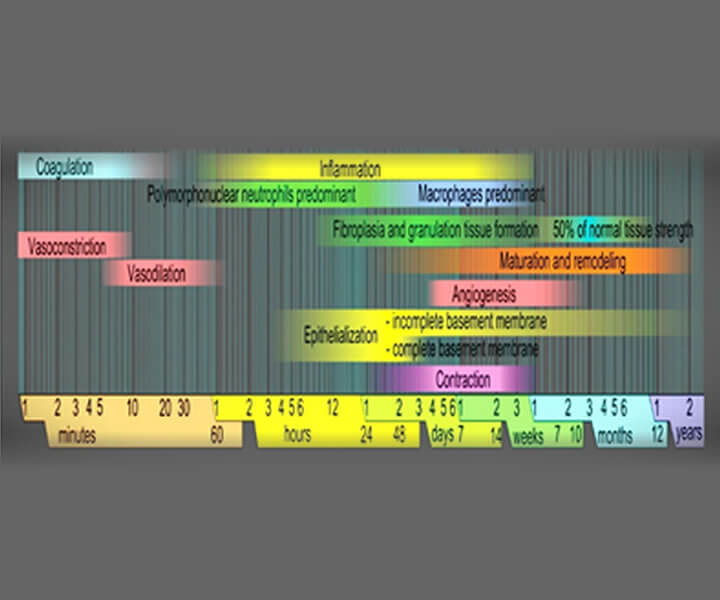
Accelerated Tissue Healing
Electrotherapy accelerates tissue healing through various mechanisms. It boosts blood flow by dilating vessels, delivering more nutrients and oxygen. It elevates cellular metabolism, promoting ATP production for tasks like collagen synthesis. Inflammation modulation is possible through cellular signaling, curbing excessive response. Electrotherapy also alleviates pain by interrupting pain signals, aiding movement and rehabilitation. Later in healing, it assists tissue remodeling by aligning collagen fibers, enhancing strength. These effects vary with techniques used. Efficacy hinges on factors like injury type, individual response, and proper professional application. intricate journey of tissue healing involves a symphony of cells, growth factors, and molecules.
Learn More
Management of Arthrogenic Muscle inhibition (AMI)
Arthrogenic Muscle Inhibition (AMI) or arthrogenic muscle response plays a role in the distinct muscular issues seen in individuals recuperating from joint injuries. If not addressed, AMI hinders immediate recovery and jeopardizes patients’ long-term joint health and well-being. Increasingly, there’s substantiating proof endorsing the application of neuromodulatory techniques to enhance muscle recuperation during the rehabilitation process. Interventions ought to be tailored to suit each patient’s requirements through collaborative decision-making between clinicians and patients. At the very least, studies suggest the maintenance of a straightforward treatment strategy by striving to promptly alleviate inflammation, pain, and swelling after the injury occurs. Current academic literature suggest that electrophysical agents (EPAs) are effective in altering arthrogenic muscle inhibition (AMI) due to its therapeutic effect of mitigating inflammation, modulating pain and decreasing joint tightness which leads to accelerated healing and improvement in functional mobility.
Learn More
Motor Unit Recruitment
Groundbreaking research delves into central and peripheral pathways in motor unit recruitment during neuromuscular electrical stimulation (NMES). Central pathways activate motor units through the central nervous system, while peripheral pathways directly stimulate muscles. NMES effects on muscle belly versus nerve trunk were compared. Stimulation site influenced motor unit recruitment. Muscle belly NMES engaged peripheral pathways, seen in M-waves; nerve trunk NMES activated central pathways, seen in H-reflexes. Nerve trunk NMES involves the central nervous system more. No torque increase or heightened central pathway activity with 100-Hz NMES was found. Unlike prior studies, no asynchronous activity was observed. NMES on both sites preserves muscle quality and reduces fatigue in rehab. Study optimizes NMES for quadriceps.
Learn More
Improving Strength through Satellite Cell Proliferation
Neuromuscular electrical stimulation (NMES) presents an intriguing approach for triggering human skeletal muscle activation, even when accomplished in a passive and localized manner. Despite its prevalent use in sports and muscle rehabilitation, there exists limited substantiation of its physiological impacts, and scanty data pertain to the rejuvenation of sarcopenic muscle in humans. Our current investigation underscores that NMES effectively incites distinct physiological cues to facilitate the regeneration of myogenic precursor cells (MPCs). This, in turn, fosters heightened fusion between satellite cells and pre-existing mature myofibers among the elderly, primarily through elevations in cytoplasmic calcium concentration. This orchestrated process seems to be underpinned by the heightened expression of myogenin, sustained by the upregulation of myo-miRNAs. These molecular adjustments are potentially facilitated by the reduction in reactive oxygen species production within the MPCs, prompted by the NMES regimen. NMES emerges as a supportive technique for enhancing muscle regeneration and augmenting the maximal isometric strength of the lower extremities in healthy elderly individuals, thereby enhancing their overall mobility.
Learn More
Resolution of inflammation
Combining manual therapy and electrotherapy decreases the concentration of pro-inflammatory mediators and improves capillary permeability, resulting in the resolution of inflammation. It warms the deep tissues, stimulates vascularity, promotes the repose of muscle tissues and stimulates drainage. Combining capacitive and resistive electrical transfer therapy (TECAR) with manual therapy enhances recovery by boosting cellular processes, natural repair mechanisms, blood flow, and pain relief. Manual therapy, using hands-on techniques, eases muscle tension, induces relaxation, and improves mobility. These combined therapies synergistically treat muscle issues effectively. Pairing manual therapy with high-intensity laser therapy (HILT) offers comparable results with less comfort. To optimize muscle disorder management, TECAR, HILT, and manual therapy together accelerate tissue regeneration, maintain elasticity, and expedite return to fitness.
Learn More